

Social support should be provided for populations with an increased risk of OHD, such as teenage mothers. Hospitalization for further care and observation is suggested for the OHD neonates. Neonatal infection was more prevalent among OHDs than for in-hospital deliveries, and the infection rate was associated with low birth weight. The OHD group comprised of more teenage mothers compared to the in-hospital deliveries category. Forty-nine (31%) OHD mothers lacked antenatal care, and 10 (6.3%) were unaware of their pregnancies. Several specific characteristics of mothers with OHDs were identified. Multivariate analysis identified low birth weight as the only factor independently associated with increased risk of infection in OHD neonates. Eight neonates in the OHD cohort had a documented infection within the first 72 hours of life, which was 11-fold higher than infections documented for the in-hospital births. Prematurity and low birth weight were significantly associated with OHD. A cohort of 158 OHD neonates was enrolled, of whom 29 (23.2%) were preterm. This study also investigated both maternal and neonatal risk factors associated with OHDs. Accidental OHDs were compared with in-hospital births, and neonatal infection was assessed. This retrospective cohort study enrolled neonates admitted at a children’s hospital in an urban setting from January 2004 to December 2017. The aim of this study was to determine the infection risk of OHDs. However, neonatal infection related to OHDs has not been studied.
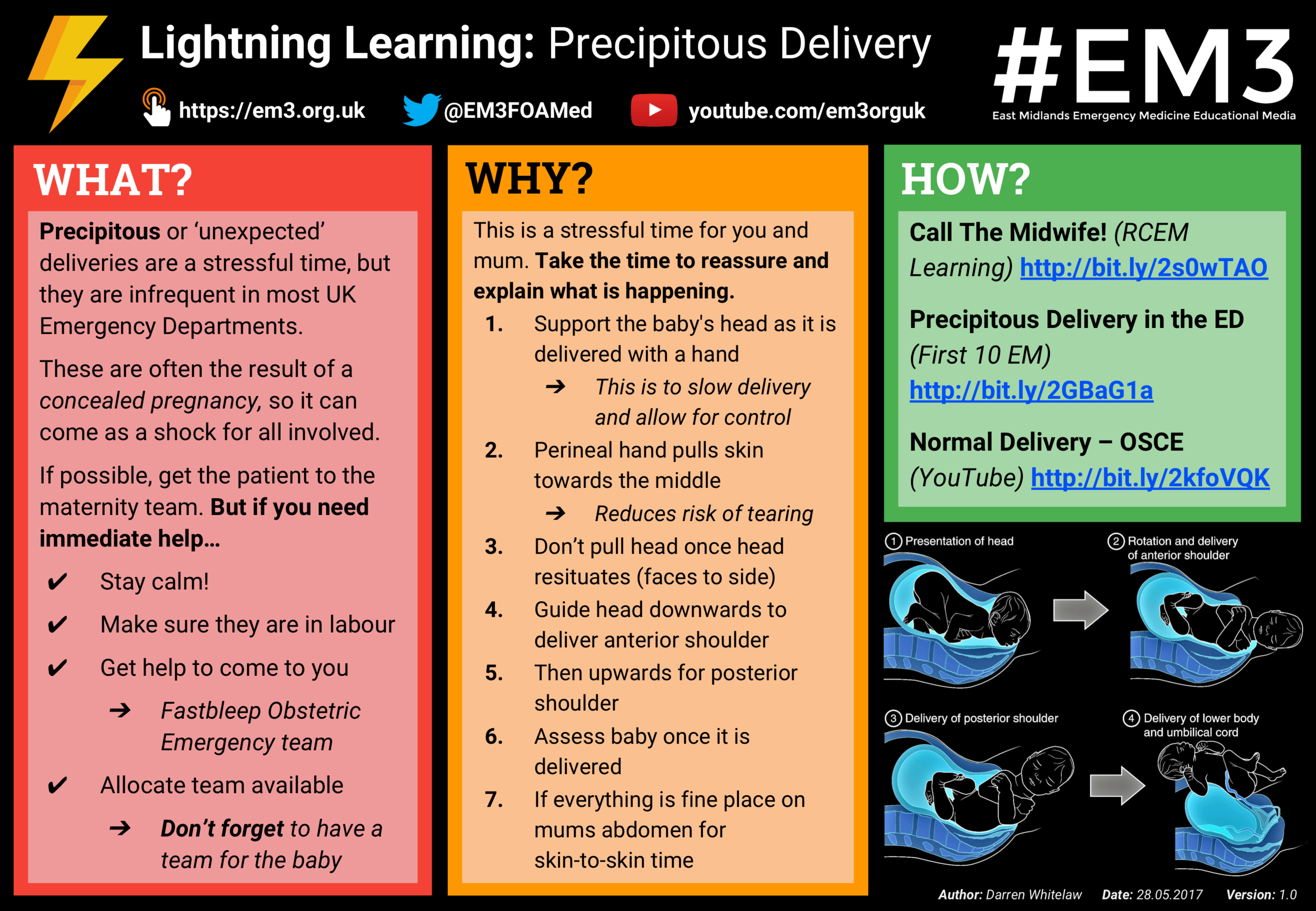

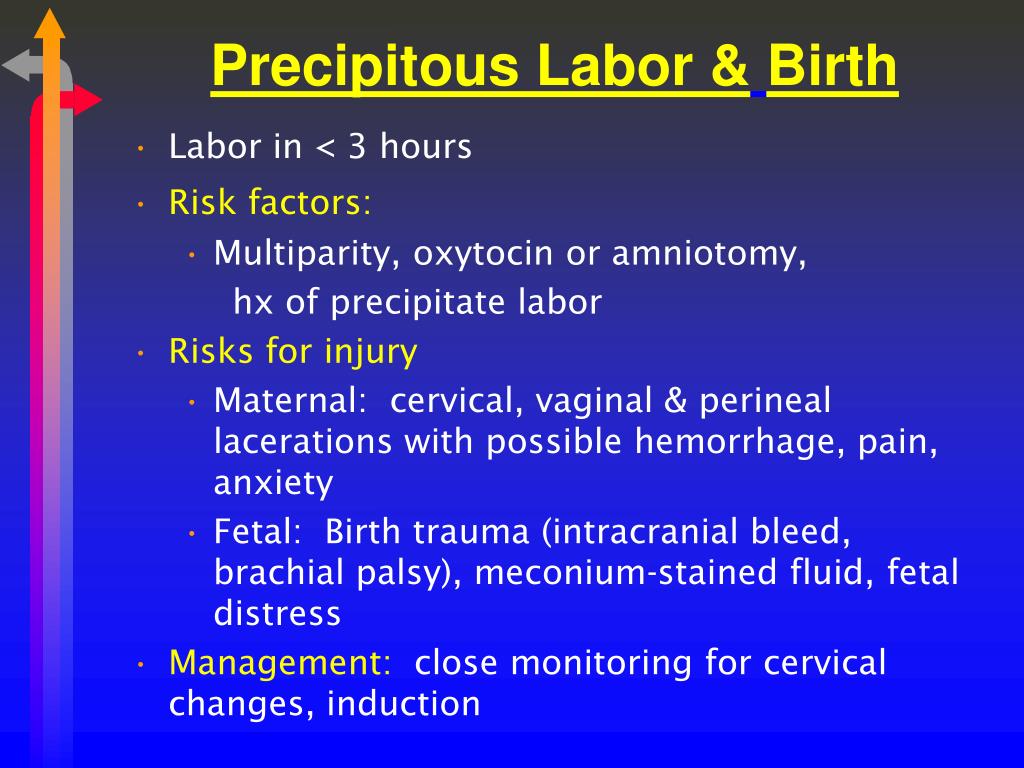
Thorough evaluation after precipitous delivery is critical to decrease maternal morbidity and mortality secondary to uterine artery injury.Īccidental out-of-hospital deliveries (OHDs) are known to have a higher incidence of maternal and neonatal complications. This seems to be the first published case report of precipitous delivery associated with uterine artery laceration and uterine rupture. Her labor course was precipitous and complicated by uterine rupture and uterine artery laceration with postpartum hemorrhage that required massive transfusion, exploratory laparotomy with a supracervical hysterectomy, and interventional radiology for uterine and cervical artery embolization. This is a case report of a 39-year-old woman, gravida 2 para 1, at 39 weeks of gestation who delivered after induction of labor due to chronic hypertension. Careful evaluation for trauma and aggressive resuscitation are critical to prevent maternal morbidity and mortality. Uterine artery laceration is a rare complication that can lead to significant postpartum hemorrhage and injury. Complications of precipitous delivery can include vascular trauma, uterine rupture, and uterine artery laceration. Precipitous delivery is associated with rapid cervical dilation and fetal descent. No significant differences were noted between the two groups regarding maternal or neonatal complications on both nulliparous and two-parous women.Īlthough precipitous labor was associated with hypertensive disorders in singleton vertex deliveries, it was not associated with maternal or neonatal outcomes. Using a multivariate analysis, precipitous labor in nulliparous women was independently associated with teenagers (adjusted OR: 1.71, 95% CI: 0.99 - 2.95, P = 0.049), preterm delivery (adjusted OR: 1.77, 95% CI: 1.16 - 2.70, P < 0.01) and hypertensive disorders (adjusted OR: 1.77, 95% CI: 1.19 - 2.65, P < 0.01), while in two-parous women, it was independently associated with hypertensive disorders (adjusted OR: 2.64, 95% CI: 1.33 - 5.24, P < 0.01). We examined the clinical characteristics and outcomes by comparing patients with precipitous labor and those with labor of normal duration in 0 and two-parous singleton pregnant women. We retrospectively examined our cases of precipitous labor to identify the clinical significance and perinatal outcomes following precipitous labor in singleton vertex deliveries.Ī retrospective population-based study was conducted comparing women with singleton precipitous labor and those with labor of normal duration. Precipitous labor is defined as expulsion of the fetus within less than 3 hours of commencement of regular contractions.


 0 kommentar(er)
0 kommentar(er)
